| Investigation |
Non-Gynae Cytology |
| Inform lab before sending |
No (unless very urgent: extension 5623) |
| Specimen type |
VARIOUS
CSF -
Obtained by lumbar puncture. Ideally, the submitting clinician should ensure a sample is submitted to clinical chemistry and microbiology as well, if appropriate. |
| Maximum Volume Required |
Pleural | 20 mls |
| Pericardial | 20 mls |
| Ascitic | 20 mls |
| Peritoneal | 50 mls |
| Synovial | 10 mls |
| Ovarian Cyst | 25 mls |
| Cerebrospinal
(CSF) | A 2 ml sample is ideal for cytology, but examination of smaller amounts can be attempted and is often successful. |
| Ureteric Washouts | 25 mls |
| Pancreatic | 15 mls |
| Cyst aspirates | Clinically benign breast cysts which aspirate to dryness, where the aspirate is not blood stained, may be discarded. Otherwise up to 20 ml of the specimen should be submitted in a sterile container. |
Specimen container
 |
Sterile 30 ml universal
Make sure lid is firmly secured |
| Transport to the laboratory |
If transport is delayed then refrigerate sample. Delays of over 48 hours are undesirable |
| Turnaround |
5 working days |
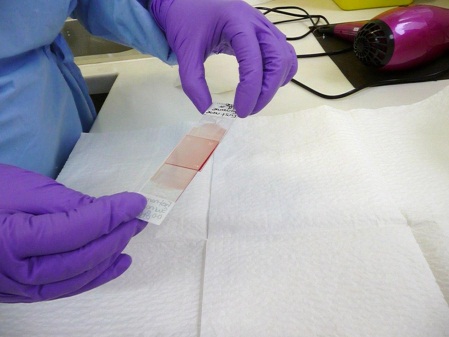
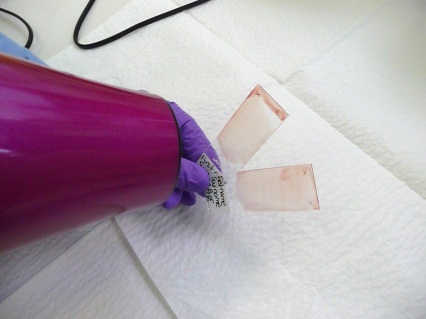
| Preparation method used by the laboratory |
Cytospin, Papanicolaou and Romanovsky May Grunwald Giemsa. |
| Factors known to significantly affect the performance of the examination or the interpretation of results |
The nature of the abnormality being investigated should be clear from the clinical information included with the specimen so that the laboratory can perform the appropriate preparations.
Imaging guidance may be required to successfully target some lesions.
A negative result of an exfoliative cytology sample is not sufficient evidence to exclude significant disease. Discussion of cases at multi-disciplinary team meetings and submission of further samples, if deemed clinically appropriate, should thus be a routine part of the diagnostic pathway. Cytology results should be correlated with histology findings. Audit against final outcomes (which may be clinical) should be performed. |
| Additional information |
Please ensure that all request forms and specimen pots are clearly labelled with patient details and relevant clinical information.
Use a Non-Gynae request form/ICE request form |